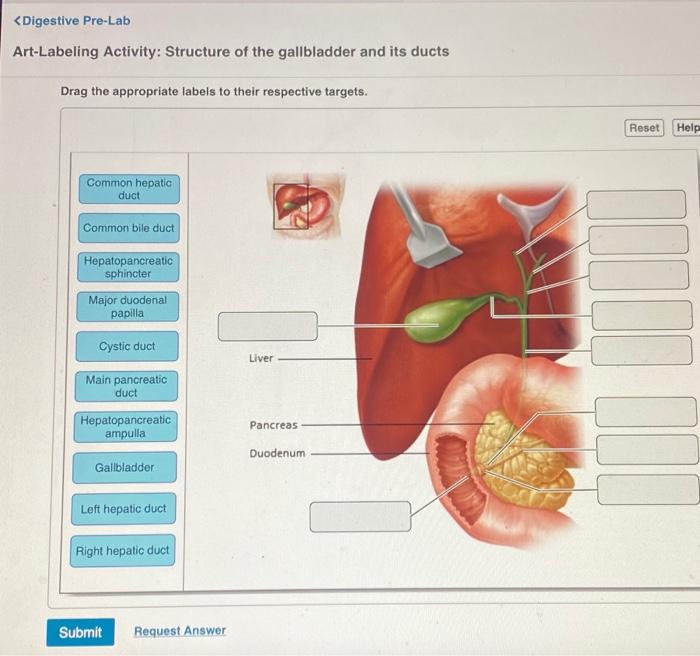
Art-labeling activity: structure of the gallbladder and its ducts – Embark on an art-labeling journey that unravels the intricate structure of the gallbladder and its associated ducts. This engaging activity not only enhances your anatomical knowledge but also fosters a deeper understanding of the biliary system’s crucial role in digestion.
As we delve into the anatomical details, you will gain insights into the gallbladder’s location, shape, and histological composition. Moreover, the interconnections between the gallbladder, liver, and bile ducts will be explored, shedding light on the seamless flow of bile.
Anatomical Structures of the Gallbladder and Ducts: Art-labeling Activity: Structure Of The Gallbladder And Its Ducts
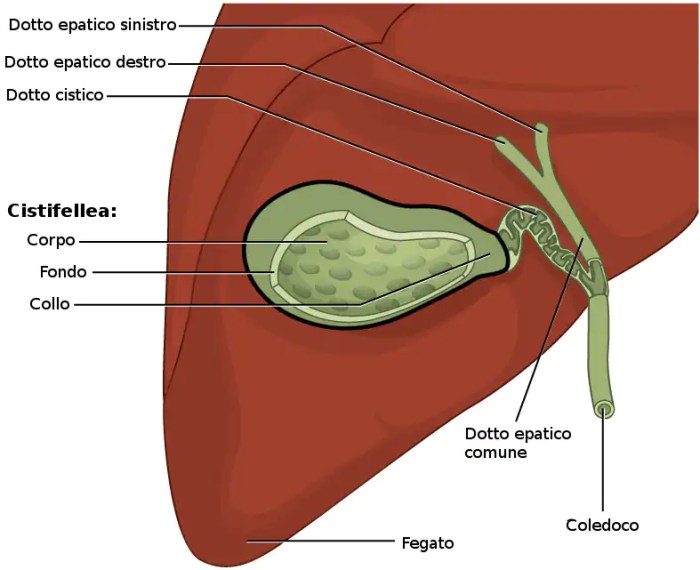
The gallbladder is a small, pear-shaped organ located on the underside of the liver in the right upper quadrant of the abdominal cavity. It is approximately 7-10 cm in length and 3-4 cm in diameter, with a wall thickness of 2-3 mm.
The gallbladder is composed of three layers: the mucosa, muscularis, and serosa.
Anatomical Relationship with Liver and Bile Ducts
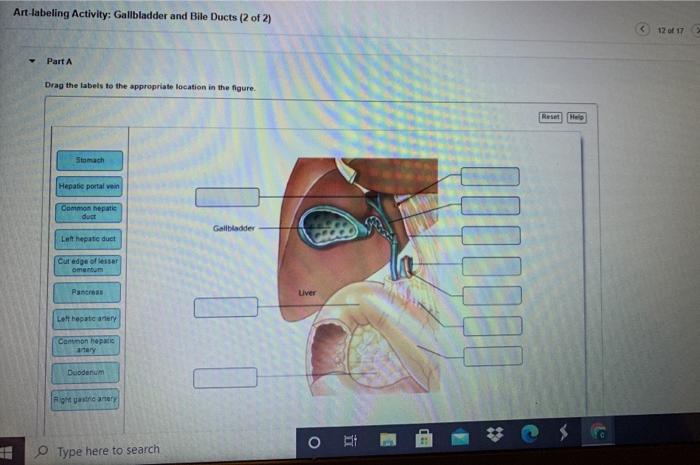
The gallbladder is closely associated with the liver and bile ducts. The liver produces bile, which is stored in the gallbladder and released into the small intestine to aid in digestion. The cystic duct connects the gallbladder to the common hepatic duct, which carries bile from the liver.
The common bile duct then joins with the pancreatic duct to form the ampulla of Vater, which opens into the duodenum.
Cystic Duct, Common Bile Duct, and Ampulla of Vater
The cystic duct is a short, narrow duct that carries bile from the gallbladder to the common hepatic duct. The common bile duct is a longer, wider duct that carries bile from the liver and gallbladder to the duodenum. The ampulla of Vater is a small, muscular sphincter that controls the flow of bile and pancreatic juices into the duodenum.
Histological Features of the Gallbladder and Ducts
Gallbladder Wall Layers
The gallbladder wall consists of three layers: the mucosa, muscularis, and serosa.
- Mucosa:The mucosa is the innermost layer and is lined with simple columnar epithelium. It contains goblet cells that secrete mucin, which protects the gallbladder from bile acids.
- Muscularis:The muscularis is the middle layer and consists of smooth muscle fibers arranged in a circular and longitudinal orientation. It allows for the contraction and relaxation of the gallbladder.
- Serosa:The serosa is the outermost layer and is a thin, transparent membrane that covers the gallbladder.
Bile Duct Histology
The bile ducts are lined with simple columnar epithelium, which is supported by a lamina propria and muscularis. The lamina propria contains blood vessels, nerves, and lymphatic vessels. The muscularis consists of smooth muscle fibers arranged in a circular and longitudinal orientation, which allows for the peristaltic movement of bile.
Comparison of Gallbladder and Bile Duct Histology
The gallbladder and bile ducts share some histological similarities, such as the presence of simple columnar epithelium and a muscularis layer. However, the gallbladder has a thicker wall and contains goblet cells in its mucosa, which are absent in the bile ducts.
Blood Supply and Innervation of the Gallbladder and Ducts
Arterial Supply
The gallbladder is supplied by the cystic artery, a branch of the right hepatic artery. The cystic artery divides into two branches: the superficial and deep cystic arteries. The superficial cystic artery supplies the serosa and muscularis, while the deep cystic artery supplies the mucosa.
The bile ducts are supplied by branches of the hepatic artery, gastroduodenal artery, and superior mesenteric artery.
Venous Drainage
The gallbladder is drained by the cystic veins, which join the portal vein. The bile ducts are drained by branches of the hepatic veins.
Lymphatic Drainage
The gallbladder and bile ducts are drained by lymphatic vessels that follow the blood vessels. The lymphatic vessels eventually drain into the hepatic lymph nodes.
Innervation
The gallbladder and bile ducts are innervated by the vagus nerve and celiac plexus. The vagus nerve provides parasympathetic innervation, while the celiac plexus provides sympathetic innervation.
Imaging Techniques for Gallbladder and Ductal Visualization
Ultrasound Imaging
Ultrasound imaging is a non-invasive technique that uses sound waves to create images of the gallbladder and bile ducts. It is commonly used to diagnose gallstones, cholecystitis, and other gallbladder and ductal diseases.
Computed Tomography (CT) and Magnetic Resonance Imaging (MRI)
CT and MRI are cross-sectional imaging techniques that provide detailed images of the gallbladder and bile ducts. CT uses X-rays, while MRI uses magnetic fields and radio waves. These techniques are useful for diagnosing more complex gallbladder and ductal diseases, such as tumors or strictures.
Endoscopic Retrograde Cholangiopancreatography (ERCP), Art-labeling activity: structure of the gallbladder and its ducts
ERCP is a procedure that combines endoscopy and fluoroscopy to visualize the gallbladder and bile ducts. A thin, flexible tube is inserted into the mouth and advanced through the esophagus, stomach, and duodenum to the ampulla of Vater. Dye is then injected into the bile ducts to make them visible on X-ray images.
Comparison of Imaging Techniques
- Ultrasound:Non-invasive, widely available, but operator-dependent.
- CT and MRI:More detailed, but more expensive and invasive.
- ERCP:Invasive, but allows for therapeutic interventions.
Clinical Significance of Gallbladder and Ductal Disorders
Common Clinical Presentations
- Cholelithiasis:Gallstones
- Cholecystitis:Inflammation of the gallbladder
- Cholangitis:Inflammation of the bile ducts
Risk Factors and Pathophysiology
Risk factors for gallbladder and ductal disorders include obesity, high cholesterol, diabetes, and a family history of these conditions. The pathophysiology of these disorders involves the formation of gallstones, which can block the flow of bile and lead to inflammation and infection.
Diagnostic and Therapeutic Approaches
Diagnosis of gallbladder and ductal disorders is based on clinical symptoms, physical examination, and imaging studies. Treatment options include surgical and non-surgical interventions, such as cholecystectomy (removal of the gallbladder) or endoscopic removal of gallstones.
Potential Complications and Prognosis
Complications of gallbladder and ductal disorders can include pancreatitis, liver damage, and sepsis. The prognosis for these disorders depends on the severity of the condition and the timeliness of treatment.
Key Questions Answered
What is the function of the gallbladder?
The gallbladder serves as a reservoir for bile, a fluid produced by the liver that aids in the digestion of fats.
What is the significance of the cystic duct?
The cystic duct connects the gallbladder to the common bile duct, allowing bile to flow from the gallbladder into the small intestine.
How does the ampulla of Vater contribute to digestion?
The ampulla of Vater, where the common bile duct and pancreatic duct join, regulates the release of bile and pancreatic juices into the duodenum, facilitating the digestion process.